Luke Powell
LEED AP, WELL AP, IWBI COVID-19 Task Force Member
Vice President
Air Equipment Company
Disclaimer:
Please note I am not a medical professional. My degree is in mechanical engineering, not the specific ways diseases spread, nor the human body’s response to those diseases. This information is being provided as a service to Air Equipment Company partners. The information provided may not apply to all readers’ specific situation and is not a substitute for application of the viewer or reader’s own judgement or the advice of another competent professional. Air Equipment Company does not make any guarantee or warranty as to the accuracy or completeness of any information provided. Air Equipment Company disclaims liability for personal injury, property damage, or other damages or any kind, whether special, indirect, consequential, or compensatory, that may result directly or indirectly from the use of or reliance on information from the webinar/paper. The researched referenced herein is based on best available as of May 25, 2020.
________________________________________________________________________________________________________
Currently, scientists believe that transmission of the new coronavirus takes place in one of three ways:
- inhalation of liquid droplets from the coughing or sneezing of a person with the infection (droplets directly from the respiratory tract of the infectious individual to the nose, eyes or mouth of the recipient, generally over short distances, necessitating facial protection)
- close contact with a person who has the infection (Close contact involves hand transfer of contamination form hand to mouth, nose or eyes, hand washing and gloves being common controls)
- contact with surfaces that contain the virus – although this is now less likely according to the CDC
Aerosol transmission may be a fourth route of transmission – there is conflicting information on this, but there is enough evidence that we should assume that it is possible. For healthcare organizations, the CDC recommends airborne, in addition to standard (contact) and droplet precautions, for the care of COVID-19 suspected or confirmed patients. In contrast to its recommendations for healthcare, the CDC makes no mention of airborne transmission in public settings.
The environments that humans have constructed, including buildings, cars, public transportation, and other human-built spaces are where we spend 90% of our time.
Building owners and operators, designer engineers, contractors and equipment manufacturers are all thinking that same thing right now. “What can be done to control the spread of viruses in a building?”. Buildings are our first line of defense when it comes to combating COVID-19 or any other virus. People are going to be afraid to come back to buildings unless you can show they are safe. It’s all about reduction or risk, not elimination of the possibility of infection.
Current estimates of the contagiousness (known as the R0 “R naught”) of SARS-CoV-2, once estimated at 5.7 are now in the 2.0 to 2.5 range (currently 0.87 in KY, but was as high as 1.86 at times). R0 is defined as the average number of people who will contract a disease from one contagious person. For reference, measles has a famously high R0 of approximately 12 to 18, and influenza (flu) has an R0 of 1.3. However, within confined spaces, the R0 of SARS-CoV-2 has been estimated to be significantly higher (estimates ranging from 10 to 14). Anything above 1.0 means that the disease is still growing, below 1.0 means that the spread is stopping. See rt.live or current stats.
Current guidelines from the World Health Organization:
- Regularly and thoroughly clean your hands with an alcohol-based hand rub or wash them with soap and water.
- Maintain at least 1 meter (3 feet) distance between yourself and others.
- Avoid going to crowded places.
- Avoid touching eyes, nose and mouth
- Make sure you, and the people around you, follow good respiratory hygiene. This means covering your mouth and nose with your bent elbow or tissue when you cough or sneeze. Then dispose of the used tissue immediately and wash your hands.
- Stay home and self-isolate even with minor symptoms such as cough, headache, mild fever, until you recover. Have someone bring you supplies. If you need to leave your house, wear a mask to avoid infecting others.
- If you have a fever, cough and difficulty breathing, seek medical attention, but call by telephone in advance if possible and follow the directions of your local health authority.
- Keep up to date on the latest information from trusted sources, such as WHO or your local and national health authorities.
People never think of buildings as being part of a healthy lifestyle. We have to change this thinking. Depending on how a building is designed and operated, it will determine what microbes will survive and what wont. This has a direct impact on our health.
Protocols for surface cleaning and air purification practices that were once only considerations in the healthcare industry are in discussions for all buildings, including offices, restaurants, education facilities, retail spaces and even grocery stores. Shouldn’t all environments be considered “critical environments”??
It is important to understand the difference between sanitizing and disinfecting. Sanitizers reduce the number of germs on a surface whereas disinfectants kills most of them. Sanitizers usually work faster than disinfectants, which can take up 10-15 minutes to kill germs according the EPA’s website. The term hand “sanitizer” is a misnomer since its main ingredient is alcohol, which is a disinfectant. The EPA current lists 420 registered disinfectants. Only 124 of these are specific for human coronavirus. Only 19 of these 124 are common chemicals/ingredients. So read labels and go to EPA.gov to verify the validity of what you are using.
The goal of this webinar is to discuss some upgrades and technologies that may be useful for infection control in buildings.
According to the WHO, SARS-CoV-2 is not airborne (per their latest brief on the subject dated March 29th), but other experts seem to disagree. Some scientists say there is preliminary evidence that airborne transmission — in which the disease spreads in the much smaller particles from exhaled air, known as aerosols — is occurring, and that precautions, such as increasing ventilation indoors, should be recommended to reduce the risk of infection.
According to the EPA and the American Lung Association, indoor air can be up to ten times more polluted than outdoor air. That is because every building generates and then traps millions of potentially harmful airborne particles, pathogens, and gases. We breathe over 10,000 quarts of air each day. With just a little bit of attention to the systems, you can turn a sick building into a healthy building.
Indoor spaces, with limited air exchange or recycled air and lots of people, are concerning from a transmission standpoint. Any environment that is enclosed, with poor air circulation and high density of people, spells trouble. That is why HVAC systems are a factor when it comes to transmission of infectious diseases. Social distancing guidelines do not hold in indoor spaces where you spend a lot of time.
Current CDC guidelines, as they relate to modifying HVAC systems to handle the COVID-19 pandemic, state the following:
- Consider improving the engineering controls using the building ventilation system. This may include some or all of the following activities:
- Increase ventilation rates.
- Increase the percentage of outdoor air that circulates into the system.
ASHRAE has established an epidemic task force to respond to the global COVID-19 pandemic. On April 15, 2020, the following statement from the ASHRAE Epidemic Task Force was posted on their website:
On the recommendation of the ASHRAE Epidemic Task Force, ASHRAE leadership has approved the following two statements regarding transmission of SARS-CoV-2 and the operation of HVAC systems during the COVID-19 pandemic:
Transmission of SARS-CoV-2 through the air is sufficiently likely that airborne exposure to the virus should be controlled. Changes to building operations, including the operation of heating, ventilating, and air-conditioning systems, can reduce airborne exposures.
Ventilation and filtration provided by heating, ventilating, and air-conditioning systems can reduce the airborne concentration of SARS-CoV-2 and thus the risk of transmission through the air. Unconditioned spaces can cause thermal stress to people that may be directly life threatening and that may also lower resistance to infection. In general, disabling of heating, ventilating, and air-conditioning systems is not a recommended measure to reduce the transmission of the virus.
On May 7th, ASHRAE’s recommendations for reopening buildings were outlined and include the following:
- Review HVAC programming to provide flushing two hours before and post occupancies. This includes operating the exhaust fans as well as opening the outside air dampers. For buildings without the capacity to treat large quantities of outside air and when outside air conditions are moderate, open all windows for a minimum of two hours before reoccupation.
- Disinfect high-touch areas of HVAC and other building service systems (e.g. on/off switches, thermostats)
- Run the system on minimum outside air when unoccupied.
- Garage exhaust, if any, should run two hours before occupancy.
According to the April 14th publication of the ASHRAE Position Document on Infectious Aerosols:
Designers of mechanical systems should be aware that ventilation is not capable of addressing all aspects of infection control. HVAC systems, however, do impact the distribution and bio-burden of infectious aerosols. Small aerosols may persist in the breathing zone, available for inhalation directly into the upper and lower respiratory tracts or for settling onto surfaces, where they can be indirectly transmitted by resuspension or fomite2 contact.
We see that the CDC and ASHRAE recommend increasing both ventilation and filtration to reduce the risk of COVID-19 airborne transmission. While some of these recommendations may be able to be implemented with little to no effect on the current HVAC systems, it is important for a facility owner or manager to fully understand the effects these recommendations may have on their specific systems before implementing them, potentially wasting time and resources only to make their building’s interior conditions worse.
The International WELL Building Institute has also created a Task Force to help in reducing the enormous health burden from COVID-19 and other respiratory infections. Its goal is to define the critical role buildings, organizations and communities play in prevention and preparedness, resilience and recovery. The Task Force’s work will take a broad approach, considering both new and recurring infectious agents that can affect large populations. Changes to WELL version 2 will reflect recommendations from the Task Force.
The solutions discussed here today should not be taken as a solution for all situations but used as methods to mitigate the spread.
Making the wrong decisions when it comes to your HVAC system could have adverse effects (high or low humidity, temperature fluctuations, condensation on surfaces, etc.) not only to the building itself but also to the health of the occupants. It is important to factor in both short-term and long-term ramifications of any changes made.
Possible Solutions:
Increasing Outdoor Air Ventilation
For years, we have been sealing our windows shut and recirculating air in buildings in order to save energy. The result are schools and office buildings that are chronically under-ventilated. This not only gives a boost to disease transmission, but also significantly impairs cognitive function.
Many studies have shown that increasing ventilation within a building can be an effective way of reducing the potential for airborne transmission. For example, according to ASHRAE Standard 170, isolation rooms, where optimal ventilation rates are required to control spread of viruses, are designed for 12 air changes/hour, 2 of which are OA.
One model looking at how ventilation could prevent aerosol transmission, suggests that for diseases transmitted by droplet nuclei, such as infuenza, having good ventilation would be as impactful as vaccinating 50-60% of the population in a poor ventilation scenario. This statistic assumes a 60% vaccine efficacy rate, and cannot be applied universally, but does give a good idea of the potential impact ventilation could have on disease spread, if COVID-19 is in fact being transmitted through the air.
Increased OA may also mean that cooling and heating coils/burners may be undersized. If you have room in the unit, consider parallel coils & parallel filter banks if retrofitting existing AHUs.
Considerations should be made for moisture infiltration into the building. The effects of moisture within a building depends on a variety of factors, which include but not limited to, current HVAC design and operation, exterior climate conditions, construction type, and the types of building materials used.
In the winter, increased OA will also likely lead to very dry conditions, which is problematic in the height of the virus season. Humidity should always be controlled when increasing ventilation air.
In demand control systems CO2 set points should be set to 400ppm or lower to increase the delivery of outside air. Ventilation should be kept on for longer, with lower ventilation rates when people are absent. It is not recommended to switch ventilation systems off in any buildings, even those temporarily vacated, but to operate them continuously at reduced speeds.
Ventilation systems should have extended operation times. Change occupied times to start ventilation at least 2 hours before building occupancy and to continue to run 2 hours after the building is unoccupied.
In the case of any systems serving a single space, recirculation of air within that space, such as through a local fan coil unit, is acceptable if you can implement some air purification measures that will be discussed later. The primary objective is to maximize the air change rate, add in as much outside air as possible and to minimize the risk of any pockets of stagnant air. It is recommended that their fans are operated continuously because the virus can sediment in filters and resuspension boost can follow when the fan is turned on. In continuous circulation operation virus particles are more likely to be removed with exhaust ventilation.
In some cases, natural ventilation may be considered if the existing HVAC systems are not capable of increased OA. Operable windows are an easy method of natural ventilation and should be considered even if existing HVAC systems can support increased OA., but some drawbacks include:
- lack of suitability for severe climates, where the ingress of very cold air causes discomfort, condensation and high energy loss
- inadequate control over the ventilation rate, which can lead to poor indoor air quality and excessive heat loss
- varying airflow rates and patterns of airflow
- noisy and polluted locations
- cannot use heat recovery from exhaust air
- inability to filter or clean incoming air
- increased occurrence of dampness and fungal growth in humid climates
Existing Systems Capabilities
An HVAC system’s impact on virus disruption will depend on source location, strength of the source, distribution of the released aerosol, droplet size, air distribution, temperature, relative humidity, and filtration. Each system within a building was likely designed to handle a specific quantity of outdoor air ventilation per ASHRAE guidelines.
Increasing the outdoor air ventilation for a specific air handling unit (AHU) system does several things:
- Changes the mixed air temperature being delivered to the cooling coil (20% = 79/65, 40% = 83/69)
- Changes the supply air temperature leaving the AHU that is delivered into the space
- Creates excess moisture the AHU system was not able to remove, or lowers RH in the space
- Moisture levels outside of 40%-60% RH, not only makes occupants feel uncomfortable but can also lead to condensation/moisture, which can settle on various building materials and lead to microbial growth if not corrected. Or can lead to structural damage (especially wood furnishings and structures)
- Requires additional ventilation air be exhausted from the building to maintain desired pressurization, so exhaust systems need to be evaluated.
Humidity
A study on coronaviruses — using proxy viruses — found that both higher relative humidity values and higher temperatures significantly decreased viral survival. At low relative humidity [20%] and low temperatures [39 Fahrenheit] — coronavirus appears to be at its strongest, most viable point.
The proper balancing of outdoor and exhaust airflows within a space is essential in maintaining a proper indoor environmental condition for both comfort and health/safety of indoor occupants. It is important to realize that if one were to increase ventilation within a space, it creates the potential for changing the relative humidity.
As air temperature increases, so does its ability to hold more moisture. The specific amount of moisture that air can hold at a particular environmental condition is typically referred to as specific humidity. However, most people usually refer to humidity levels in a term called “relative humidity” or percent RH. Relative humidity is the amount of moisture air can hold compared to the maximum amount of moisture the air can hold at a specific temperature. For example, air at 75°F and 50% RH means the air is holding 50 percent of the total capacity of moisture it has the ability to hold while at 75 degrees.
Just as the ability to hold more moisture when air temperature is increased, if you decrease air temperature, the ability of the air at the cooler temperatures to hold moisture decreases also; however, the relative humidity actually goes up, while the specific humidity remains the same. When relative humidity reaches 100 percent, the air is considered saturated and condensation will form. The air temperature at this point is typically referred to as the “dew point” temperature. Dew point temperature is the temperature at which water vapor condenses in the air.
According to ASHRAE Standards, occupied spaces should be controlled to a maximum relative humidity level of between 55-65 percent RH. Therefore, the operation of HVAC systems should be controlled to achieve these recommended humidity levels at all times, regardless of COVID-19 or other potential similar threats, to prevent the potential for other adverse effects relating to moisture and condensation to occur. 40%-50% RH is also the optimal range to minimize human stress, which compromises the immune system.
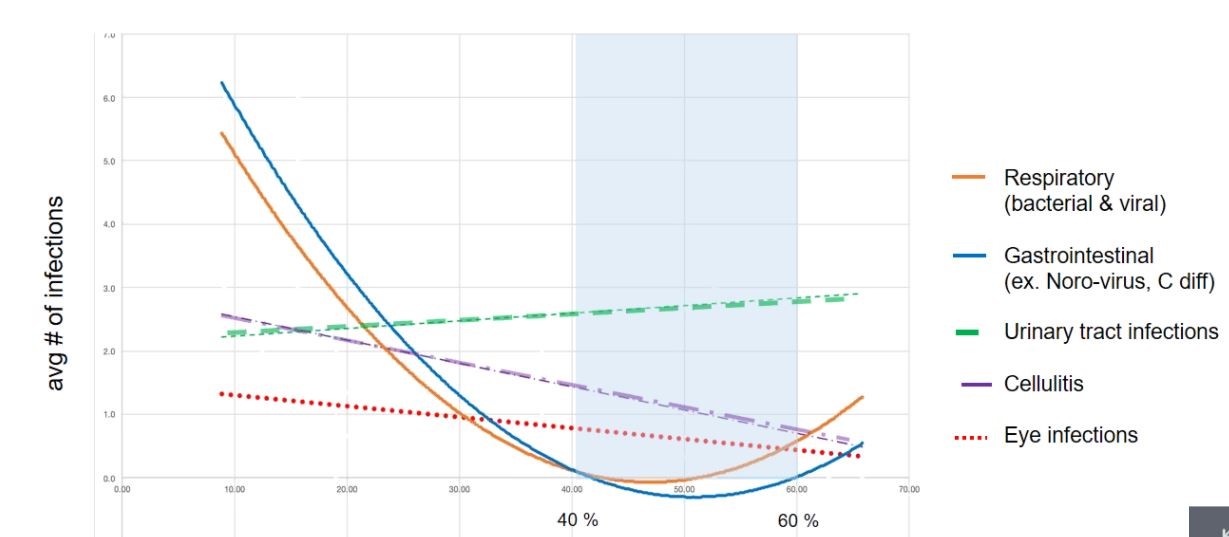
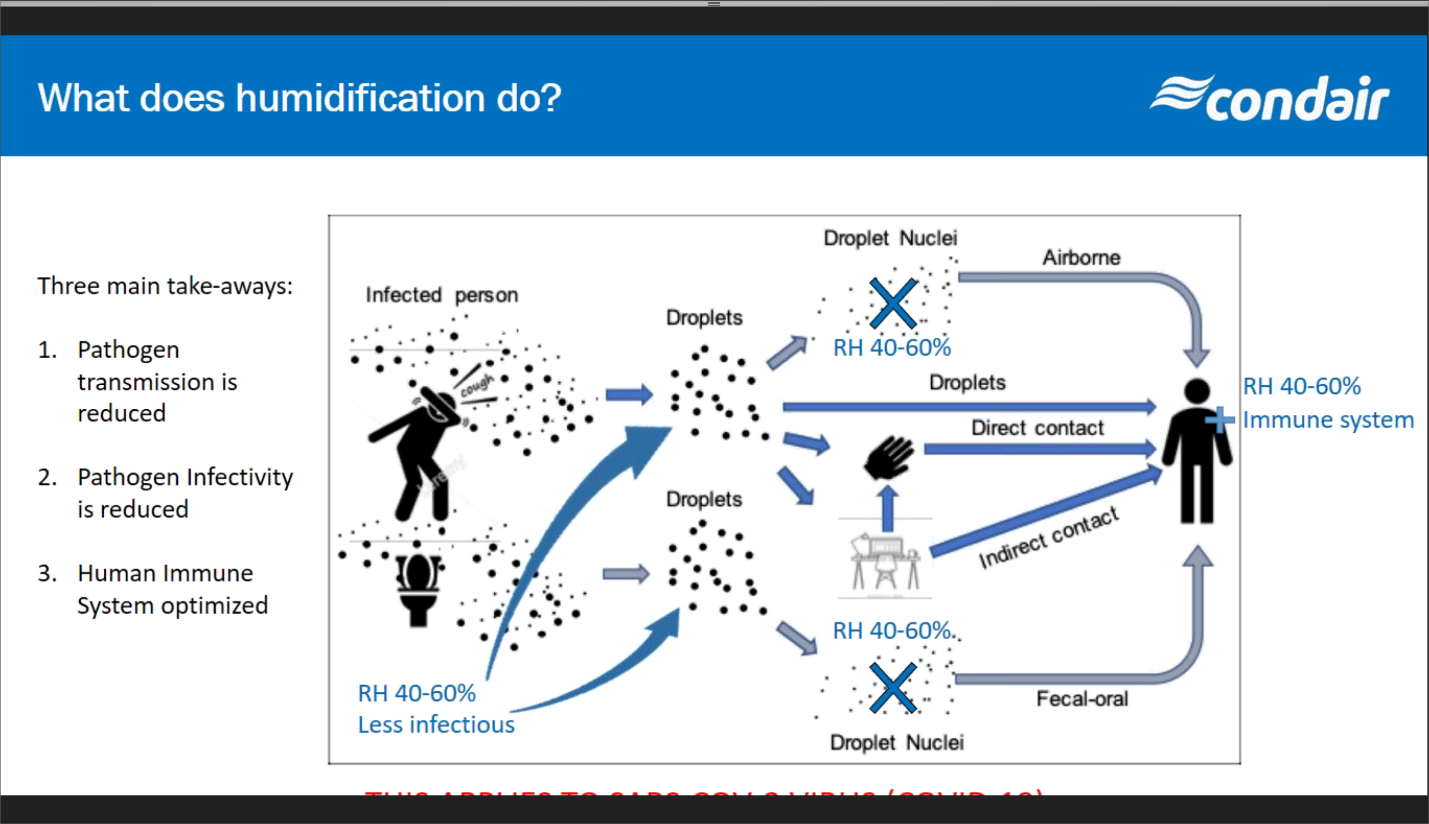
This is a study from four years in a nursing home. Patient infections show respiratory infections were high under around 42%RH and above around 52%RH. Under dry conditions, the human protective mechanisms in the airways and lungs become compromised after just 15 minutes in a dry environment and are at optimal levels at 50% RH.
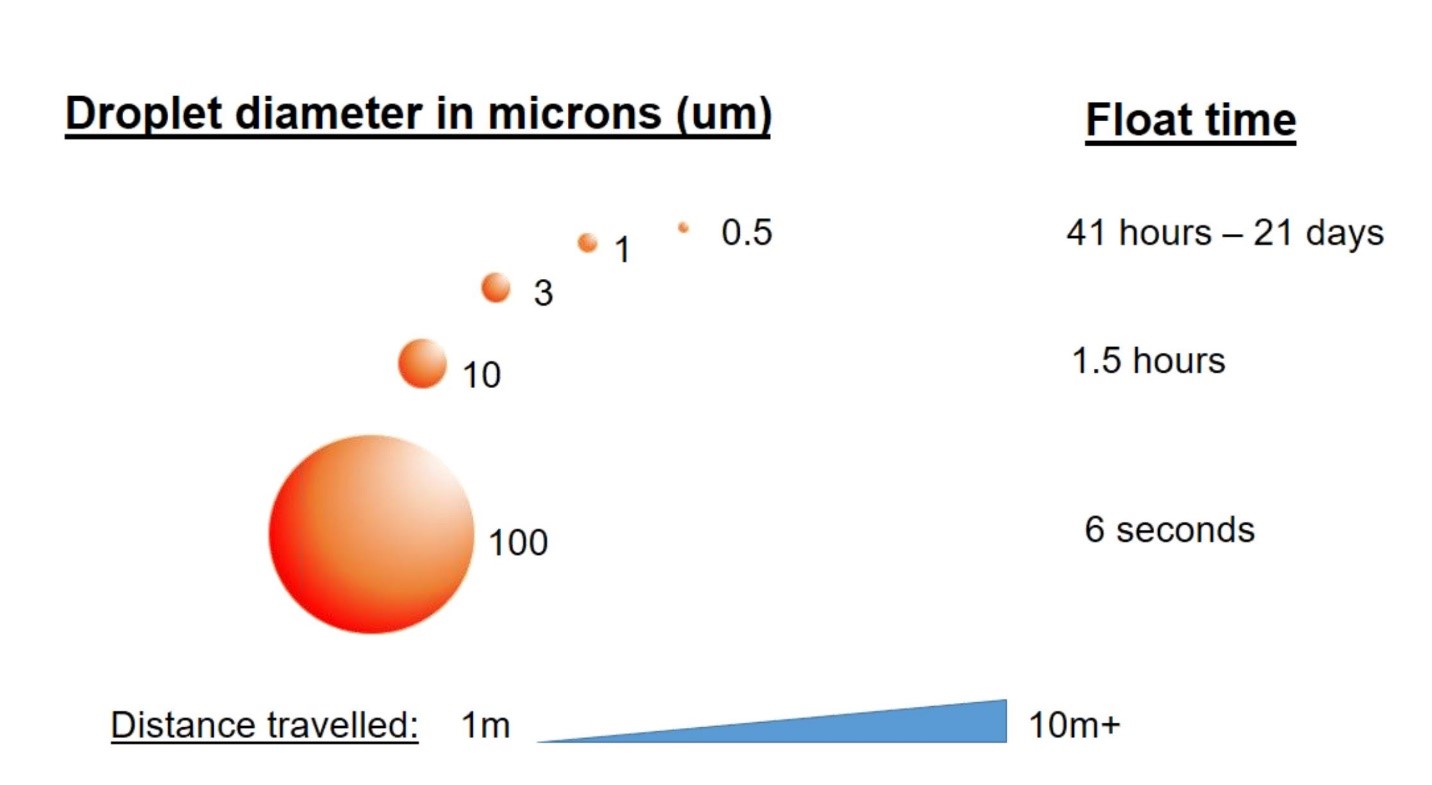
Droplets that start large, will shrink in dry environments, allowing them to stay airborne longer. By maintaining indoor relative humidity between 40–60%, building operators can reduce the risk of spreading airborne infectious diseases in their facilities. Think of droplets like snow. Big snowflakes are heavy and stay in place once they land. Light snowflakes they are drier are easily blown around by the wind and are harder to keep from blowing back on your driveway, sidewalk or car windshield.
Pathogens and infectious droplets travel further in dry air, especially when the relative humidity is below 40%, which is partly why we tend to see more illness in the drier winter months. The relative humidity of most homes and buildings during the November-March period falls below 35% and on occasion below 25%. That environment is very conducive for viral transmission.
In most climate zones across the U.S., maintaining this range throughout the year requires not only the dehumidification technologies (cooling coils) that are traditionally designed in HVAC systems, but also the less common technologies that add humidification (steam generating humidifiers) to spaces.
Mount humidifier upsteam of cooling coil (will act as a mist eliminator), but at a minimum before the fan. You will get some heat gain from the fan and come off of the saturation line. If the air is saturated when it hits the filter, it will degrade the filter if the humidifier is installed immediately upstream of the filter.
Increasing Filtration
Upgrading AHU filter efficiency is an effective way to assist in removing unwanted airborne particles. However, careful consideration needs to be made when selecting the types of filters used for existing AHU systems. In general, higher MERV filters capture more and smaller airborne particles.
The HEPA designation (MERV 17-20) means that the filter assembly was designed and tested to capture 99.97% of particles in the air passing through it. If aerosol transmission is confirmed, HEPA filters will be very effective in capture airborne coronaviruses.
The virus that causes COVID-19 is approximately 0.125 micron (125 nanometers) in diameter. It falls squarely within the particle-size range that HEPA filters capture with extraordinary efficiency: 0.01 micron (10 nanometers) and above. Many media outlets and competing technologies have incorrectly stated that HEPA filters don’t filter below 0.3 micron and therefore could not capture airborne coronaviruses. That is incorrect. HEPA filters are actually most efficient at capturing ultrafine particles below the 0.3-micron HEPA test standard. HEPA filters can be very effective in capturing and removing viruses from air streams, as long as they pass through the filter. In general, while highly effective and reliable, an in-duct HEPA filter is more appropriate in preventing cross contamination between spaces than it is in guaranteeing removal of contaminants from a given space.
The American Society for HealthCare Engineering (ASHE) tells us that a MERV 16 rated filter has 95% or better efficiency for particles of 0.3 to 1.0 micron sizes, and due to Brownian motion (the erratic random movement of microscopic particles in a fluid, as a result of continuous bombardment from molecules of the surrounding medium) particles smaller than 0.3 microns are trapped within filter media just as efficiently as those of the 1.0 to 0.3 micron size. They state that “MERV 16 is effective in capturing the SARS-CoV-2 virus”. ASHRAE recommends upgrading filters to MERV-13 or the highest level achievable. MERV 13 rating that can be installed in an existing filter rack as MERV 16 and higher are usually a 4” or 5” wide filter and MERV 13 can be 1” or 2”. The MERV rating is the initial rating of the filter, the MERV A is the rating for the life of the filter.
Both ventilation and filtration are code mandated requirements in hospitals as well as other buildings, and it is the careful implementation of both these approaches that may garner the best result.
Considerations regarding increased filter efficiency:
- Increased resistance or static pressure within a system
- All filters have specific pressure drops associated with them, which varies depending upon the type of the filter itself as well as the quantity of airflow across it. Pressure drops also increase as the filters become dirty. Installing a higher efficiency filter may work fine initially while the filter is clean but may not when the filter gets dirty, as the AHU fan may then be outside its performance range, resulting in a decrease in total airflow. Therefore, one needs to analyze the AHU system to determine if the system can accommodate a higher efficiency filter.
- Simply increasing the speed of the fan or even the horsepower (hp) of the fan motor may make up for the added pressure drop within the system. However, for smaller AHU systems, such as those found in most residential, multi-family, and light commercial buildings, the installed AHU systems likely do not have these capabilities due to the size and hp limitations of the supply fans themselves.
- Lowering the airflow and therefore velocity across the filter bank will help capture smaller particles from the airstream (due to Brownian motion), but this may negatively impact comfort control and coil performance. Most commercial filters are tested at 492 fpm. Filters perform differently at different airflow velocities.
- Drop in total airflow being delivered to a space
- Lower velocity across a cooling coil could lead to coils freezing up.
- Filters are only good at capturing what is in the airstream of the AHU. Airflow patterns must carry contaminants to the filter. Small particles like viruses circulate in the room for an extended time before eventually making their way to the filter for capture.
- Gaps around filters are common. Holding frames with gaskets are the most effective at minimizing bypass around the filters.
It is important to have each system evaluated by a licensed mechanical engineer or vendor familiar with such systems before any changes to the systems are made. This may include verifying the AHU system performance by a licensed test and balance or mechanical contractor to assure the system is performing in accordance with its intended design standards — and also to verify what, if any, excess capacity the respective systems have before making temporary or permanent changes to their current operation.
Bipolar ionization
Bipolar ionization generators create positively and negatively charged oxygen ions which bind to contaminants in the indoor air, either causing them to drop out of circulation in the room where they cause the most problems for occupants or to be captured by a filter within an AHU. Must be positive and negative ions, not just negative. Make sure they generate 1000-1200 ions per cm3. When ions attach to airborne pathogens, such as viruses, they cause a chemical reaction on the surface of the cell membrane. This deactivates the viruses, rendering them harmless, so they can no longer spread or cause infection.
Independent lab tests have shown that these bipolar ionization systems can reduce dust and mold, capture odors, reduce VOCs (volatile organic compounds), and reduce viruses and bacteria in the air. A test against the Influenza A (H1N1) virus showed that when the viruses was introduced in a test chamber with circulating air (uncertain of air flow rate), the needlepoint ionization generator reduced 86.6% of H1H1 virus after one hour.
These ions have a relatively short lifespan (30 seconds to 15 minutes), so for them to work, you have to pass air over the ion generator consistently to ensure sufficient contact. Typically, bipolar ionization generators are installed in the ductwork, a terminal unit in the zone or directly in the air handling unit, but stand-alone recirculating room units are available through some manufacturers.
Pros of these systems are that they create little to no additional pressure drop in the system and they do not require any changes to other systems in the building. They also help control TVOC, particles, odors, dust, mold and pollen.
With any ionization product, it is important to investigate the potential to create ozone, which has proven negative effects on human health. Make sure that products adhere to zero ozone emissions as defined by UL. The needlepoint style generators can emit very low doses of ozone, but always ask to see a manufacturer’s ozone concentration test as performed by an independent lab. Glass tubes, known as corona discharge tube DO create ozone at small levels.
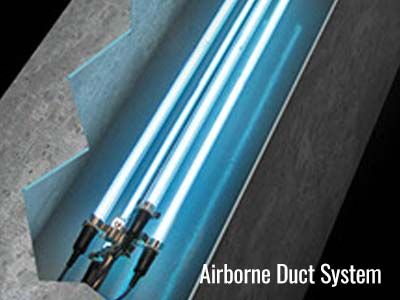
UV Light
Ultraviolet light mangles the genetic material in pathogens — called DNA in bacteria and fungi and called RNA in viruses — preventing them from reproducing. Most UV systems are tested and validated against bacteria, viruses, mold & fungus.
There are a number of factors that need to be addressed in order to determine efficiency, these include but not limited to:
- The application, such as surface or air disinfection
- Air velocity and temperature
- Recirculation rates
- Dwell time
- Specific biological target
Every organism has a Dose Effect (officially called Fluence). The Dose Effect = Time x Intensity. If an organism is on a surface, you have plenty of time (up to the point it replicates) to dose it and deactivate. For surface applications, with a given Dose Effect, the Intensity of the UVGI (Ultraviolet Germicidal Irradiation) system can be minimal given the Time variable is greater. For an airstream decontamination the Intensity needs to be greater (more lamps) because the Time variable is much smaller. UV systems are installed in the HVAC unit and/or ductwork and are designed to disinfect surfaces and the air as it circulates through the ventilation system. Installed in the AHU, it keeps the walls, evaporator coil and drain pan disinfected. They are normally installed downstream of the cooling coil in the direction of airflow. This is favored because the air downstream is saturated and drain pans are often extended in this location to catch raw water carry-over. The installation of lamps downstream of filters is generally recommended as well in order to keep them as clean as possible. If duct airstream treatment is desired, the UV bulbs can be installed parallel to the direction of airflow and can be designed in a grid with up to 6 lamps to maximize exposure based on number of passes the air will take over the lights. A wavelength between 200–280 nm (nanometers) has proven to be the most effective for infection control. UV-C fits in this range.
Every microorganism requires a specific UVC dosage for inactivation, including coronavirus. UV disinfection has been employed for decades in water treatment; these microwatt values have been used for reference to gauge UVC efficiency against a large cross-section of microorganisms. While UV systems have not been specifically tested against this coronavirus, they were tested against SARS. In a 2004 study, exposure of the virus to UVC light (254 nm emitted 4016 μW/cm2) resulted in partial inactivation at 1 min with increasing efficiency up to 6 min, resulting in a 400-fold decrease in infectious virus.
UV disinfection systems for room, surface & HVAC are an ideal proactive measure to complement filtration.
While most products provide their wavelength — which, ideally, should be around 260 nanometers (nm) — most don’t provide their irradiance, which tells you how long it will take to kill a coronavirus.
Unlike bipolar ionization, the light does not travel through the system or space. UV-C can only decontaminate air that passes through it. It is also good at removing particulates, TVOCs and bacteria.
There are also applications of “in-room” UV sterilizers specific to almost every application, including stationary lights or portable devices mounted on robots for off hour surface sterilization. It is important that these are sized correctly for the room as many do not have the flow rate to be effective in larger spaces. Portable ultraviolet units are already being used to sterilize surfaces in hospital rooms and subway cars, but these can be used only when those spaces are unoccupied due to the damage UV-C can do to skin.
Another option is known as Upper-Room UV, where fixtures are mounted on walls or ceilings, similar to fluorescent lights used today, which would shine ultraviolet light across the top of an interior space, well above people’s heads. Ceiling fans would be installed to draw air upward so that floating bacteria, viruses and fungi are zapped more quickly.
LED using the UVA-Violet spectrum is new, and has benefits
- Lasts up to 5 years
- Not harmful for humans
But it does not have the power of UVC-Filament Quartz Lamps. UVC-Filament lamps are still recommended for HVAC, except for Mini-Splits, where LED is preferred, due to the limited space.
Photocatalytic air purifiers also use UV light. The catalyst that cleans the air is typically titanium dioxide and it is energized by ultraviolet UV light. The big advantage that photocatalytic air purifiers have over other air-cleaning technologies, such as filters is that instead of simply trapping pollutants, they completely transform the harmful chemicals and effectively destroy them. The disadvantage of this process is that photocatalytic purifiers can also produce tiny amounts of ozone (O3), well within the guideline limit (0.05 parts per million) suggested by the US FDA but, even so, this is something to bear in mind. Instead of removing TVOCs completely, a photocatalytic air purifier may chemically convert them into other unpleasant pollutants, including formaldehyde and acetaldehyde.
Sunlight also produces UV Light. Ultraviolet-C plays a significant role in viral inactivation as we have discussed. However, UVC rays from the sun do not reach the Earth’s surface because they are completely absorbed by the atmosphere. Ultraviolet B and A, which do penetrate the atmosphere, can inactivate viruses as well, but to a lesser extent. Higher sun angle increases receipt at ground level, increasing viral inactivation. Thus, the most favorable time for viral inactivation is between May and September in the Northern Hemisphere. A combination of fresh air and sunlight seems to have prevented deaths among patients during the 1918 Spanish Flu.
ASHRAE does not make a recommendation for or against the use of UV energy in air systems for minimizing the risks from infectious aerosols, but Centers for Disease Control and Prevention (CDC) has approved UVGI as an adjunct to filtration for reduction of tuberculosis risk and has published a guideline on its application.
Active particle control devices
Active particle control devices perform similarly to a bipolar ionization generator, with one important distinction. Rather than charging oxygen molecules to act as a contaminant attraction device, active particle control devices charge the contaminant particle itself, causing it to aggregate with other smaller particles to form a larger conglomerate particle that can be captured by a downstream air filter. These devices effectively increase the filtration ability of the downstream filter by grouping smaller particles together. This technology has been used for years in clean rooms and operating rooms.
Through electrical field control and placement techniques, it can convert a low particle capture efficiency filter into a high capture efficiency one. The smallest particles, too small to be captured by the MERV 15 equivalent collector, pass through the device’s energy field and are conditioned, making them “net neutral”. They are then sent back out into the air space. Each of these can attract other smaller particles that have an opposite charge. As a result, every net neutral particle works both as a powerful magnet to attract other ultra-fine particles, and as an absorbent sponge, soaking up oppositely charged VOCs.
They have the same advantage as bipolar ionization in that they add little additional pressure drop added to system. These air purifiers can be installed in air handler filter racks or as portable in-room units. They do require some maintenance and calibration. Typical cartridges can hold from 6 to 12 months of contaminants before needing to be replaced. They will obviously also cause filters to load up faster.
Dynamic Air Cleaners is another technology that use electrostatic attraction to polarize contaminates in the air so that they stick together more readily.
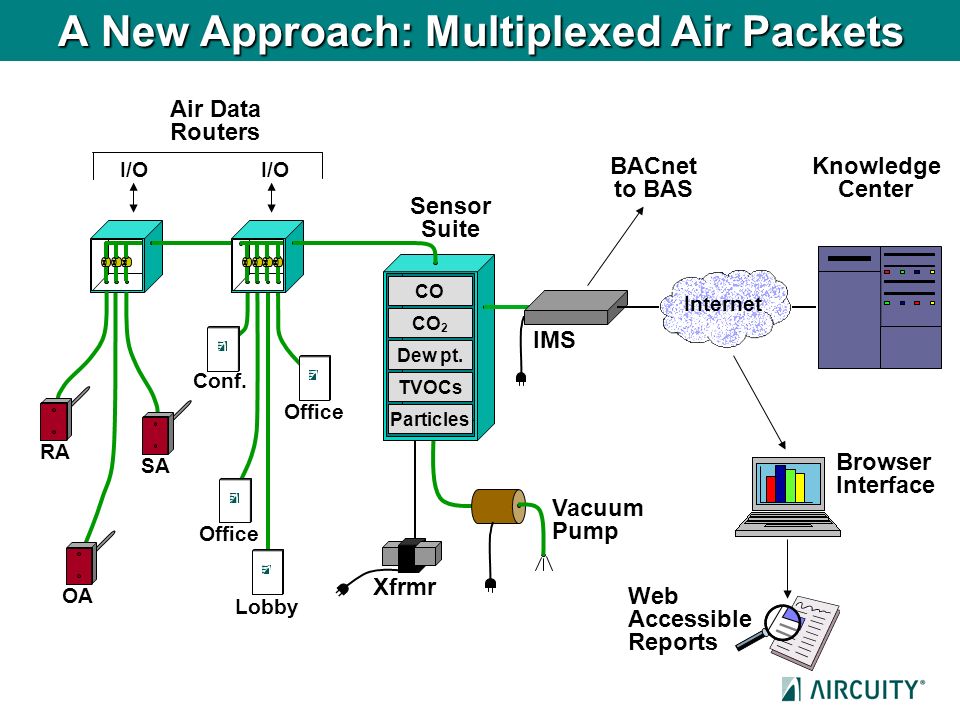
IAQ Monitoring
It is hard to determine if some of these technologies are working unless you are measuring contaminants in the air. IAQ Monitoring Systems can measure and control variables to verify that other solutions are working through live monitoring over internet and through BMS.
Monitoring Humidity is important to verify that you are in the proper range (40%-60%RH) for health, comfort and building structural integrity.
When increasing ventilation air, using Demand Control Ventilation is an effective way to assure that energy is not wasted. DCV can control OA levels based on building occupancy (CO2 levels or occupancy sensors) in order to control energy usage.
Many studies have confirmed a link between ambient particulate matter (PM2.5) and chronic conditions. PM2.5 is particulate matter that has a diameter of less than 2.5 micrometers, which is about 3% the diameter of a human hair. PM2.5 exposure affects overall health of immune system including but not limited to chronic airway inflammation and an increased risk of developing a respiratory infection. It can be safely argued that regions of the world that have a significant problem with air pollution in the form of particulate matter, and in particular PM2.5, have very strong correlation to areas gravely affected by the coronavirus pandemic.
PM2.5 dust is very dangerous for our health. It is perceived as especially damaging because it can accumulate deep in the lungs and penetrate other organs and the bloodstream, causing a serious threat to health. Adding small particle measurement to the airstream for both pre and post side of the filter banks and looking differentially at space increases in particle levels is the best method for understanding and remediating high particle levels.
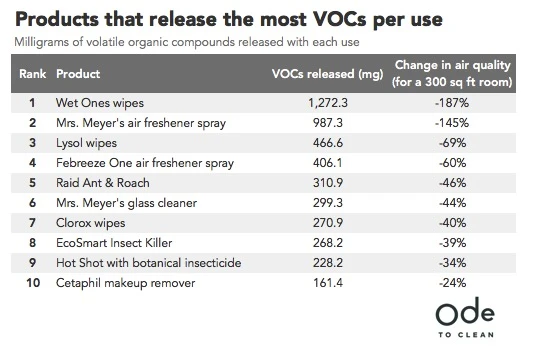
Increased use of disinfectant and sanitizing products will lead to higher levels of TVOCs in the indoor environment. IAQ monitoring of these compounds can be critical to overall health of the occupants. Building operators need to know where and when the VOC’s are in high concentration in the indoor air and adjust ventilation to those spaces to keep air clean and healthy.
These particles, CO2, humidity and TVOC sensors and systems must be maintained (calibrated every 6 months) to assure accuracy. They can be hand-held (will need a separate sensor for each parameter) or a system that takes air samples back to a centralized location with multiple sensors.
Other Considerations
Where cleaning or planned maintenance of ventilation systems is required, it should be undertaken with care. Appropriate PPE should be worn and all materials, including old filters, should be carefully bagged and disposed of safely.
Room air cleaners, that integrate a multilayer pre-filter, electrostatic precipitator, HEPA filter, activated carbon filter, UVC lamps, photo-catalytic oxidizer, and a bipolar ion generator all in one might be a good option. But their clean-air delivery rate (~350 cfm) when converted to room ACH is often trivial—no more than 1 or 2 added ACH for anything larger than a small office.
Future design/construction considerations
- An increase in disinfecting and sanitizing in buildings will lead to a spike in TVOCs. Monitoring these levels should be considered as even at low levels they can cause headaches and nausea, as well as eye, nose, and throat irritation. Certain VOCs have been linked to the development of allergies and asthma.
- Increased prefabrication offsite – lesson the number of workers on sites
- Remote access to all BMS monitoring and data
- Virtual Commissioning
- Who is responsible for the health of the employees?
- Who is responsible for the health of the building?
- Empower someone in the company to take responsibility of the health of the building and its occupants
- There needs to be a Chief Wellness Officer.
- We are going to have shift back to buildings that are built for health. The energy crisis of the 1970’s moved us away from this into energy efficient buildings limiting OA. Make decisions that go beyond code minimum.
- Healthy Building Movement was already happening, but COVID-19 has put it on fast-forward.
- Planetary Health and Human Health can and must coexist.
- We must turn building IEQ parameters into business benefits to eliminate any barriers to adopt this strategy
- We need to understand the value-added chain of decision makers. It starts with investors, but building occupants are now starting to drive some of these decisions.
- Demand must come from the public to change things and encourage designers to go well beyond what regulations and code calls for.
- Buildings will need to have a scorecard to let occupants know what is being done/tested in the building
- Develop messaging and education for building occupants—dashboards, apps, situational cues—to reduce concerns regarding potential pathogen transmission.
- A combination of several of these solutions, such as improved media filtration combined with UVGI or Bi-Polar Ionization is probably the only way to really ensure you are scrubbing the air effectively.
- Increasing the amount of ventilation in the space and controlling humidity may the best long-term solution for the health of building occupants. There is a potential penalty for every change to the system or sequence of operations, weigh the pros and cons of each before implementation. There is no one size fits all.
Final Thoughts:
I think we can all agree that it is likely that the new coronavirus will be a lingering part of life well into next year, but we should not have to be shut down in quarantine or even follow the strict social-distancing measures that were needed this time around. We can control the spread in the future by making buildings healthier.
In the future, COVID-19 may become like the common flu is today—a recurring menace of winter. Right now, that seems like a wonderful place to be. I believe we can get there by rethinking the built environment and how to interact in it and with it. The importance of the spaces where we live, work, study, and play has shifted dramatically.
As we are now moving toward reopening and living with COVID-19, we have to shift and become a more resilient society—and the buildings and public places we inhabit will play a critical role in this shift.
Thank you for your time today. Any of us here at Air Equipment Company will be happy to discuss your specific needs and applications at any time, so just reach out.
REFERENCES:
https://www.esmagazine.com/articles/100389-dr-stephanie-taylor-petitions-the-who-for-40-60-rh-policy
https://www.erinbromage.com/post/the-risks-know-them-avoid-them
https://www.ansys.com/about-ansys/covid-19-simulation-insights
https://www.cushmanwakefield.com/en/news/2020/04/how-to-guide-for-reopening-workplaces-released
https://www.nature.com/articles/s41586-020-2271-3
https://kshe.org/page/webinars
https://www.ashrae.org/file%20library/about/position%20documents/pd_infectiousaerosols_2020.pdf
https://www.epa.gov/report-environment/indoor-air-quality
https://www.ashrae.org/about/news/2020/ashrae-offers-covid-19-building-readiness-reopening-guidance
https://www.ncbi.nlm.nih.gov/books/NBK143277/
https://thewirecutter.com/blog/can-hepa-air-purifiers-capture-coronavirus/
https://blog.plasma-air.com/plasma-air-kills-airborne-viruses-cleaning-the-air-you-breathe/
https://www.lenntech.com/library/uv/will1.htm
https://www.epa.gov/radtown/ultraviolet-uv-radiation-and-sun-exposure
https://www.theatlantic.com/health/archive/2020/03/how-will-coronavirus-end/608719/
https://www.explainthatstuff.com/how-photocatalytic-air-purifiers-work.html
https://airqualitynews.com/2020/04/09/why-air-pollution-is-linked-to-a-faster-spread-of-coronavirus/
https://www.aircuity.com/blog/3195/
https://www.nytimes.com/2020/05/07/science/ultraviolet-light-coronavirus.html
http://www.centerforactivedesign.org
https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2#filter_col1
https://pubmed.ncbi.nlm.nih.gov/15350737/